A newly identified link between chronic pain and lung cancer in a pre-clinical model offers hope for pain management
Pain is an important alarm system engineered to provoke rapid withdrawal from harmful situations.
But for hundreds of millions of people, the alarm bells keep going off long after healing from an initial injury. Persistent pain may arise in the absence of stimulus, injury, or disease. Despite its prevalence, chronic pain is among the least well-managed and least understood areas of healthcare.
Better ways to control pain are urgently needed, especially in light of an opioid crisis that claimed 75% of the half a million deaths attributed to global drug overdoses in 2021 alone1. The way out is clear: there must be alternatives to opioids in the form of novel drugs based on a fundamental understanding of their underlying mechanisms.
A new study published today in Science Translational Medicine points to possible new treatments for chronic pain, with a surprising link to lung cancer. The work was spearheaded by LSI Director Dr. Josef Penninger and Dr. Clifford Woolf, professor of neurology and neurobiology at Harvard Medical School and director of the F.M. Kirby Neurobiology Center at Boston Children’s Hospital, along with researchers from IMBA – Institute of Molecular Biotechnology of the Austrian Academy of Sciences.

Dr. Shane Cronin
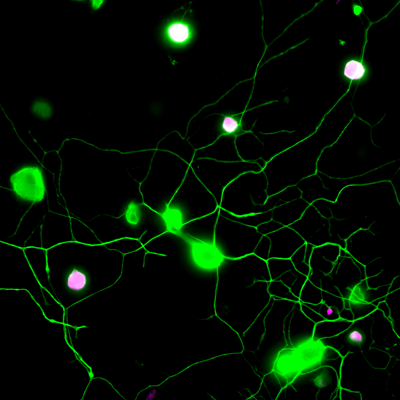
“We had previously shown that sensory neurons produce a specific metabolite, BH4, which then drives chronic pain, such as neuropathic pain or inflammatory pain,” says project lead and co-corresponding author Dr. Shane Cronin, a staff scientist in the Penninger lab at IMBA and a former postdoc in the Woolf lab at Harvard Medical School and F.M. Kirby Neurobiology Center, Boston Children’s Hospital. “The concentrations of BH4 correlated very well with the pain intensity. So, we naturally thought that this was a great pathway to target.”
To identify drugs that reduce BH4 levels in pain neurons, the researchers performed a “phenotypic screen” of 1000 target-annotated, FDA-approved medications. This approach allowed the scientists to start their search using medications that are currently in use for various indications, and to identify undescribed, off-target analgesic properties. Among the first findings of this hypothesis-driven search, the team was able to link the previously observed analgesic effects of several drugs, including clonidine and capsaicin, to the BH4 pathway.
“However, our phenotypic screen also allowed us to ‘repurpose’ a surprising drug,” says Cronin. The drug ‘fluphenazine’, an antipsychotic, has been used to treat schizophrenia. “We found that fluphenazine blocks the BH4 pathway in injured nerves. We also demonstrated its effects in chronic pain following nerve injury in vivo.” The researchers also found that the effective analgesic dose of fluphenazine in their experiments in the mouse model is comparable to the low end of the doses safely indicated for schizophrenia in humans.
Dr. Clifford Woolf
In addition, the screen uncovered a novel and unexpected molecular link between the BH4 pathway and EGFR/KRAS signaling, a pathway involved in multiple cancers. Blocking EGFR/KRAS signaling reduced pain sensitivity by decreasing the levels of BH4. The genes of EGFR and KRAS are the two most frequently mutated genes in lung cancer, which prompted the researchers to look at BH4 in lung cancer. Surprisingly, by deleting an important enzyme, GCH1, in the BH4 pathway, the mouse models of KRAS-driven lung cancer developed fewer tumors and survived much longer. The researchers uncovered a common signaling pathway for chronic pain and lung cancer through EGFR/KRAS and BH4, thus opening up new avenues of treatment for both conditions.
“Chronic pain is currently subjected to often ineffective palliative treatments. Furthermore, effective painkillers such as opioids can lead, if used inappropriately, to severe addiction. It is therefore critical to find and develop new and repurposed drugs to treat chronic pain,” says co-corresponding author Dr. Clifford Woolf, professor of neurology and neurobiology at Harvard Medical School and director of the F.M. Kirby Neurobiology Center at Boston Children’s Hospital.
One intriguing aspect of the study is the mechanistic link between pain and lung cancer. “The same triggers that drive tumor growth appear to be also involved in setting the path to chronic pain, often experienced by cancer patients,” adds co-corresponding author Dr. Josef Penninger, who is the founding director and currently a group leader of IMBA in addition to serving as the Scientific Director of the LSI. “We also know that sensory nerves can drive cancer, which could explain the vicious circuit of cancer and pain. Understanding this cross-talk is not only critical for cancer treatments, but might also help to improve the quality of life for cancer patients towards less pain.”

Dr. Josef Penninger
Original publication:
Cronin, S. J. F., et al., “Phenotypic drug screen uncovers the metabolic GCH1/BH4 pathway as key regulator of EGFR/KRAS-mediated neuropathic pain and lung cancer”. Science Translational Medicine, 2022. DOI: 10.1126/scitranslmed.abj1531
1 https://www.who.int/news-room/fact-sheets/detail/opioid-overdose
About the LSI:
The Life Sciences Institute (LSI) at the University of British Columbia conducts basic research aimed at improving human and planetary health. As a Global Research Excellence Institute, the LSI is home to the Biological Resilience Initiative, which integrates foundational trans-disciplinary research across multiple scales to shed light on the mechanisms of resilience in biological systems.
Within this approach, our 20 multidisciplinary research focus teams pursue collaborative discoveries in diabetes, cardiovascular disease, antimicrobial resistance, infectious disease, cancer biology, developmental disorders, environmental microbiology and more.
About IMBA:
IMBA – Institute of Molecular Biotechnology – is one of Europe’s leading biomedical research institutes. IMBA is located at the Vienna BioCenter, the vibrant cluster of universities, research institutes, and biotech companies in Austria. IMBA is a subsidiary of the Austrian Academy of Sciences, the leading national sponsor of non-university academic research. The stem cell and organoid research at IMBA are being funded by the Austrian Federal Ministry of Science and the City of Vienna.
Contact
Bethany Becker
Communications Manager
UBC Life Sciences Institute
Tel: 604-838-4585
Email: bethany.becker@ubc.ca
Daniel F. Azar, PhD
Communications Officer
IMBA – Institute of Molecular Biotechnology, Vienna, Austria
Tel: +43 1 79044-3821
Email: daniel.azar@imba.oeaw.ac.at