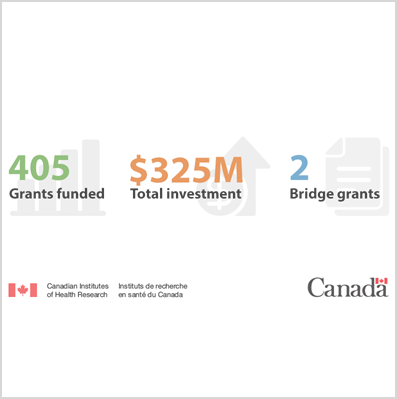
Congratulations to the successful applicants in the CIHR Spring 2022 Project Grant competition!
Listed below are the PIs on the ten funded projects. LSI Director Dr. Josef Penninger and Deputy Director Dr. James Johnson described the results as a remarkable success: 42% of the LSI applications were approved, whereas the Canadian national and UBC averages are 19% and 22%, respectively.
“This is a great testament to our thriving research community and the great work that is done at all levels,” they said, “from grant development support by Richa Anand and Nina Maeshima to the technology core support to – of course – all the great research work and ideas that are the key and foundation to this success.”

A specialized neural circuit representing novelty on behavioural timescales

Determining the role of FMRP complexes in autism-relevant gene expression
Mutations in the gene FMR1 lead to disorders that are associated with intellectual and reproductive impairment. This includes fragile X syndrome, which is the most common cause of autism. The FMR1 gene encodes a protein FMRP which regulates the translation (protein production) of other genes in the brain and reproductive tissues. When mutated, this regulation is disturbed, and many autism-relevant genes become expressed at lower levels than normal. The loss of FMRP leads to severe intellectual disability, as well as impaired sperm and egg development. Despite considerable effort, little is known about how FMRP promotes the translation of its targets. We have developed a new system for discovering the details of this process taking advantage of the accessibility of the oocytes of the model organism Drosophila melanogaster. We have used this system to identify for the first time partner proteins that work with FMRP to promote autism-relevant gene expression. This proposal aims to understand how these proteins work with FMRP to promote autism-relevant gene expression, with the goal of opening up new avenues for the development of treatments for autism patients.
Behaviour-based cell separation to interrogate host cell heterogeneity in CAR-T cell therapies
Chimeric antigen receptor cell therapy is a new form of cancer therapy that modifies a patient’s own immune cells in order to give them the ability to eliminate cancer cells. These therapies have been shown to be highly effective against certain cancers. A major challenge in the continued development these therapies is that most of the modified immune cells do not participate in the killing of tumor cells as intended. This variability increases the potential for side-effects, as well as higher dosage requirements that results in greater cost. In order to determine why only some of the modified immune cells are functional, we are developing a technology to separate cells based on behaviour observed under a microscope. Using this technology, we will separate cells that function efficiently in tumor cell killing in order to study them in isolation to determine molecular basis that drive their function. This capability will reveal potential approaches to improve the design of these therapies to improve outcomes for patients by reducing side-effects and dosage requirements.

The cell is surrounded by a lipid membrane and contains multiple, distinct organelles, also surrounded by membranes. Different organelles contact each other, forming nanometer (nm)-scale membrane contact sites observed by electron microscopy. Below the ~250 nm limit of visible light to distinguish between two adjacent objects (diffraction barrier), these contacts are therefore difficult to visualize by conventional fluorescence microscopy. Applying machine learning to super-resolution fluorescent microscopy, that breaks the diffraction barrier, we developed approaches to study contacts between two organelles: the endoplasmic reticulum, responsible for the synthesis of cellular proteins, and mitochondria, which generates the energy required for cellular function. Our focus is a protein called Gp78, which induces the formation of a distinct type of mitochondria-endoplasmic reticulum contact (MERC) and also induces the endoplasmic reticulum to engulf damaged mitochondria, resulting in the destruction of the engulfed mitochondria. This latter process, called mitophagy, is important as it destroys damaged mitochondria which produce oxygen radicals harmful to the cell. We will study how Gp78 regulation of MERCs and mitophagy may prevent progression of a cancer to malignancy. We will use our novel super-resolution imaging analysis approach to identify the contacts where Gp78, and other proteins, mediate physical interaction between endoplasmic reticulum and mitochondria. We will also test how loss of these proteins and contacts impacts mitochondrial health and behavior and extend these studies to cells in tumors to determine how these mechanisms affect tumor cell production of harmful oxygen radicals. We will define the mechanisms by which Gp78 induces MERCs and mitophagy and test whether targeting these mechanisms impacts tumor cell production of oxygen radicals.

In humans, storing too much body fat leads to a higher risk of developing heart disease and type 2 diabetes. For a long time, researchers have known that men and women store fat differently in their bodies, and also have a different risk of developing heart disease and type 2 diabetes. Unfortunately, most studies aimed at figuring out ways of correcting excess body fat to prevent heart disease and type 2 diabetes do not include both men and women. This is a problem because drugs used by doctors to fix excess fat storage do not work equally well in both men and women. To develop better treatments for people with too much body fat, researchers will need to learn more about how men and women store fat differently. My lab uses the fruit fly to make basic discoveries about fat storage. Scientists have shown that the same factors control body fat in flies and humans. Also, male and female flies store fat differently, just like in humans. These similarities mean that studying flies is a great way to learn more about how males and females store fat differently. Our research in flies shows that males and females store fat differently mostly because of one cell type in the brain called a neuron. Specifically, we found that different genes act in neurons in males and females to control body fat. This means the genes that act in neurons to control body fat are not shared between males and females. Our project goal is to identify genes that act in male and female neurons, respectively, to control body fat. Then, we will carry out tests to find out how these genes change neuron function, how the changes to body fat come about (ex. shifts in eating or movement). By providing reliable information about which genes act in neurons to control body fat in males, and which genes do the same job in females, researchers will have important clues to choose good targets for new drugs aimed at treating heart disease and type 2 diabetes in men and women, respectively.


Structural and functional investigation of Junctophilins in health and disease

François Jean
Pre-clinical development of broad-spectrum antiviral strategies against human respiratory viruses of pandemic concern
Respiratory viruses such as SARS-CoV-2 (the virus causing COVID-19) and Influenza A virus, have inarguably had an enormous impact on human health. Although vaccines have greatly limited COVID-19 and Influenza-related hospitalizations and deaths, these viruses are continually changing, resulting in decreased effectiveness of vaccines over time. Drugs that can prevent and treat infections caused by respiratory viruses are therefore also needed. Our research teams have discovered an exciting drug that can block infections caused by multiple viruses, which we call “broadly acting antivirals”. The drug, N-0385 blocks a human protease (a protein that cuts other proteins) that viruses, such as SARS-CoV-2 and Influenza A virus, take advantage of to enter the cells in our respiratory tract. In this research proposal, our aims are to further improve the pharmaceutical properties of N-0385 lead drugs, so they are more stable, easier to deliver and more suitable for animal and human drug trials. We will then measure how well these improved drugs can block SARS-CoV-2 and Influenza A virus infection in lung and other respiratory cell models when given alone or when combined. Overall, we anticipate that this research will advance these compounds so they can be further tested in clinical trials and in the future will lead to new and exciting therapeutic avenues for treatment of viruses with human pandemic potential.
Development of LNP/mRNA systems for direct transfection and generation of functional Chimeric Antigen Receptor (CAR) T-cells in-vivo for treatment of blood and other cancer cell types
Chimeric Antigen Receptor (CAR) T cell therapy is relatively new and exciting form of cancer therapy which uses a patients own re-programmed immune cells to specifically target and destroy cancer cells. In this treatment, T cells (a type of immune cell) are harvested from a patients blood and re-programmed in a laboratory to express a protein called a Chimeric Antigen Receptor, which enables them to recognize and destroy specific types of cancer cells. These CAR T cells are then re-infused into the patient where they attack and destroy the cancer cells, which can result in disease remission. Several treatments have been approved by the FDA to date. The current methods of generating CAR T cells in the lab involve genetic manipulation using viruses, and the engineered cells are not the same as natural T cells, which can cause significant problems in patient treatment; further, harvesting the T cells from blood is expensive and arduous for the patient. Here, we propose to deliver the instructions for T cells to make a CAR directly in the body by using lipid-nanoparticle(LNP)/CAR-mRNA complexes, similar to the current COVID-19 mRNA vaccines. By optimizing the composition of these LNP/mRNA complexes, it is possible to enable mRNA delivery to specific tissue and cell types. The objective of these studies is to develop a method for delivery of CAR mRNA directly to T cells via lipid-nanoparticle based delivery, potentially removing significant treatment barriers to patients.